Lead Poisoning
- What is Lead Poisoning
- "Safe" Blood-Lead Levels
- Lead in the Body
- Lead Affects Health
- References
Its use in gasoline for highway travel was first restricted with the introduction of cars requiring catalytic converters that needed lead-free gasoline, followed by the rapid phasedown on January 1, 1984, and finally a total ban on January 1, 1995. Lead additives are still used in aviation fuel. The lead from mining, smelting, lead-based paints, and gasoline contaminated household dust and outdoor soil.
Lead used to make pipes and solder contaminates drinking water. Other sources of lead include lead-glazed pottery, some metal jewelry and even cosmetics. Breathing air, drinking water, eating food or ingesting dust or soil that is contaminated with lead can cause many health problems. In adults, lead increases blood pressure and causes infertility, nerve disorders, muscle and joint pain. It can also make a person irritable and affect their ability to concentrate and remember. Lead is especially dangerous for children. Their vulnerability is related to their need for minerals to support development plus their common hand-to-mouth behavior, especially during infancy. Children swallowing even small amounts of lead may develop anemia, severe stomachache, muscle weakness and brain damage. Exposure to tiny amounts of lead are linked to lower IQ scores.
Advisory Committee on Childhood Lead Poisoning Prevention.
Low level lead exposure harms children: a renewed call for primary prevention.
US Department of Health and Human Services, CDC, Advisory Committee on Childhood Lead Poisoning Prevention; 2012.
Centers for Disease Control and Prevention.
Response to Advisory Committee on Childhood Lead Poisoning Prevention recommendations in Low level lead exposure harms children: a renewed call for primary prevention.
US Department of Health and Human Services; 2012, MMWR 61(20):383.
Analytical capability for measuring lead has played a critical role in understanding the hazards of exposure to lead. As analytical skills improved, new findings about the health hazards of different levels of exposure became evident. The health outcomes associated with various blood lead levels triggered actions to prevent exposure. Over the decades the evolution of CDC blood lead guidelines closely tracks the analytical capability for measuring blood lead. Thus during the 1960’s reliable measurements of blood lead were extremely high at 60 µg/dl. With major improvements in analytical capabilities, in 1970 the “acceptable lead exposure” declined to 30 µg/dl etcetera.
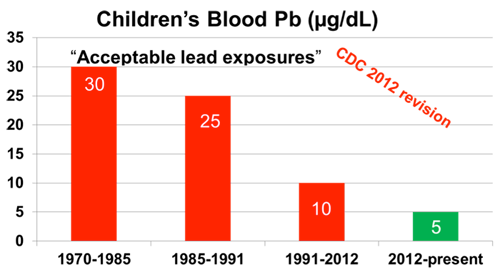
The research community has observed that blood lead levels of 2 µg/dl and even lower are associated with various chronic diseases, learning and behavioral issues. In 2012, CDC supported the research community by making two critical changes. First it recognized that there is no known minimum level of lead exposure which can be defined as safe. And secondly CDC guideline language about children’s “acceptable lead exposure” was revised to “reference value”. The revision is feasible because it is now possible to reliably measure blood lead levels at 1 µg/dl and even lower. The reference value is connected to the findings of the 97.5th percentile of the National Health and Nutrition Evaluation Survey (NHANES) results for children’s blood lead in the U.S. Currently the top 2.5% of the children in the U.S. have a blood lead level of 5 µg/dl or higher. The NHANES is repeated every few years and because blood lead is declining the future blood lead reference value should also decline.
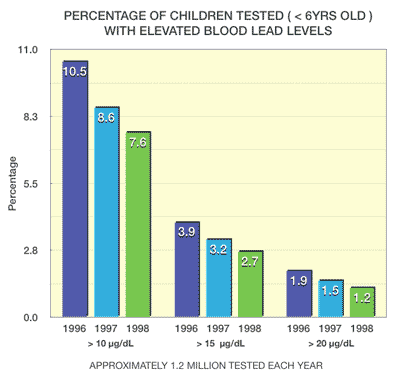
Overall, blood-lead levels are falling in the United States and this is a remarkable achievement brought about by improved engineering and chemical changes in both paints and gasoline. Looking back, we see that between 1976 and 1980, 9 out of every 10 one- to five-year-olds had lead levels greater than 10 µg/dl. Between 1988 and 1991, the same blood lead levels were detected in only one out of every 11 children. All-in-all, the average blood-lead levels for all age groups dropped over 90% since the late 1970s.
The decreases are credited to the government mandated removal of lead from gasoline, paint, food and drinking containers, eliminate lead from plumbing systems as well as increased education and awareness about lead. The most effective steps involved changes in technology that removed lead from products and the environment.
Even though blood-lead levels in U.S. children dropped between 1976 and 2012, many children, especially minority, low-income and urban youth, still face lead poisoning because of hazardous lead contamination of their environment. The main hazards are associated with the legacy of the massive use of lead by our society during the twentieth century, and this legacy plays out in communities surrounding former lead smelters and in cities such as Atlanta, Baltimore, Boston, Chicago, Detroit, Philadelphia, and New Orleans.
In the body, lead enters the bloodstream (99 percent is associated with red blood cells and 1 percent is in the plasma) where it is carried throughout the body. Lead meets one of two fates: 1) It can be excreted through the kidneys or intestines; or 2) It can be stored in soft tissue and bones and teeth where it is slowly released over decades.
 More than 95 percent of total lead in the adult body is in bones and teeth. Throughout a lifetime, lead is mobilized back into the bloodstream in times of stress, chronic disease or pregnancy/lactation (a hazardous exposure source for unborn fetuses).
More than 95 percent of total lead in the adult body is in bones and teeth. Throughout a lifetime, lead is mobilized back into the bloodstream in times of stress, chronic disease or pregnancy/lactation (a hazardous exposure source for unborn fetuses).
Even though single exposures are hazardous, it is chronic exposure that poses the biggest threat. Constant, long-term exposure from both the external environment and total body burden (all lead circulating or stored in a body) can cause adverse health effects. For instance, even if a person is removed from a lead source and blood-lead levels return to normal, the stored lead can be mobilized for decades, representing a continuous lead source that could cause lead poisoning.
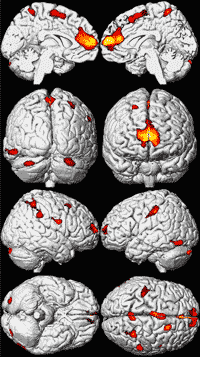
Figure 1. Regional Brain Volume Loss for the Cincinnati Lead Study Participants show more A composite representation of regions with significant volume loss for male and female CLS participants (n = 157) associated with mean childhood blood lead concentrations is shown with red and yellow clusters overlaid upon a standard brain template (seen at multiple angles; the first row presents views from the midline of the left and right hemispheres, respectively; the second row demonstrates views from the back and front of the cerebrum, respectively; the third row shows the lateral right and left hemispheres; and the fourth row shows views from below and above the cerebrum.
Brain template source reference [51]. doi:10.1371/journal.pmed.0050112.g001.
 Lead affects almost every bodily system, but susceptibility varies with age, gender and nutritional status.The element affects the nervous system and kidneys, inhibits hemoglobin production, interferes with vitamin D's duties in cell maturation and skeletal growth, affects fetal development and may cause renal cancer.
Lead affects almost every bodily system, but susceptibility varies with age, gender and nutritional status.The element affects the nervous system and kidneys, inhibits hemoglobin production, interferes with vitamin D's duties in cell maturation and skeletal growth, affects fetal development and may cause renal cancer. Most vulnerable are unborn babies and young children. The heavy metal can damage growing brains and nervous systems that have not yet formed their natural protection systems. Unborn babies are exposed through their mother's blood. Through hand-to-mouth action, children from nine months to 6 years-years-old inadvertently eat lead in paint, dust or soil. They can absorb and retain up to 50% of the swallowed element.
Once in the body, children's health effects vary. With severe lead poisoning, problems range from permanent mental retardation to death.
Figure 1. Blood Lead Levels in Young Children ( USA & Selected States, 1996--1999 ). Centers for Disease Control and Prevention (CDC), MMWR.
Lower blood-lead levels also create a range of problems including a drop in IQ. One study found blood-lead levels of 10 µg/dl lowered IQ by 3 to 5 points. Additionally, constant exposure to low lead levels causes attention deficit, hearing loss, slowed growth, headaches and hyperactivity.
Some of these illnesses go unnoticed until a child first attends school. By that time, the irreversible brain damage may be enough to interfere with life-long learning. Adults who live or work with high amounts of lead also suffer. Related health problems include difficulties during pregnancy, reproductive problems, muscle and joint pain, digestive problems, memory and concentration problems, nerve disorders and high blood pressure.
Centers for Disease Control and Prevention 2014 MMWR: Lead Screening and Prevalence of Blood Lead Levels in Children Aged 1–2 Years — Child Blood Lead Surveillance System, United States, 2002–2010 and National Health and Nutrition Examination Survey, United States, 1999–2010
- Update: blood-lead levels - United States, 1991-1994. 1997. Morbidity and Mortality Weekly Report. Department of Health and Human Services, Centers for Disease Control and Prevention. 46(February 21):141-146.
- Lead Toxicity: Case Studies in Environmental Medicine. 1992. Agency for Toxic Substances and disease Registry, U.S. Department of Health and Human Services. Publication 099-3380. 30 pp.
- Blood levels keep dropping - New guidelines proposed for those most vulnerable. Department of Health and Human Services, Centers for Disease Control and Prevention, National Centers for Environmental Health, Childhood Lead Poisoning Prevention. (February 21, 1997 press release).
- Centers for Disease Control. 1991. Preventing lead poisoning in young children: a statement by the Centers of Disease Control. Atlanta, GA:Department of Health and Human Services.
- Meadows, R. 1996. Growing pains. Environmental Health Perspectives. 104(February):146-149.
- From a speech at Earth Day 1997 at the Center for Bioenvironmental Research at Tulane and Xavier Universities in New Orleans, Louisiana.
- Cleanup and lawsuits proceed in an old Idaho mining valley. Washington Post. May 5, 1997: A1,A13.








